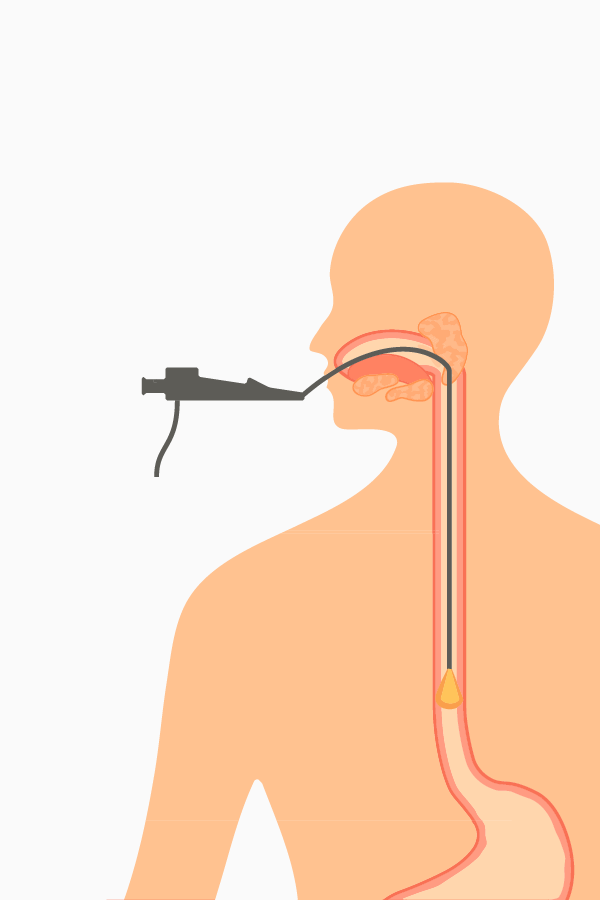
The diagnosis of eosinophilic oesophagitis (EoE) is confirmed by histology in a patient presenting with oesophageal dysfunction and specific oesophageal features. An endoscopy is not diagnostic, but can increase the suspicion of EoE in a patient with dysphagia or food bolus obstruction, which must then be confirmed histologically.
The typical clinical symptoms in adults with EoE are dysphagia and food impaction as well as heartburn, regurgitation (during or immediately after eating), and/or chest pain.1 (see table 1).
Validated questionnaires for use in EoE patients can aid in qualifying disease activity and its impact on the patient’s quality of life.2–5

-
Adults
- Dysphagia
- Bolus obstruction
- Retrosternal chest pain
- Abdominal pain
- Heartburn
- Regurgitation (during or immediately after eating)
To avoid symptoms while eating, many patients develop adaptive strategies or behaviours such as:
- Chewing slowly
- Drinking copious amounts of liquids or adding liberal amounts of sauce to foods while eating
- Avoiding certain foods
- Avoiding social situations involving food due to fear of choking in public
Physicians should therefore ask patients targeted questions about their eating habits to enable an adequate assessment of the extent of the symptoms. This can be helpful to establish a baseline before starting a treatment in an EoE patient, from which to reference when evaluating the potential impact of the treatment on these behaviours. Click here to find out more about the symptoms of EoE.
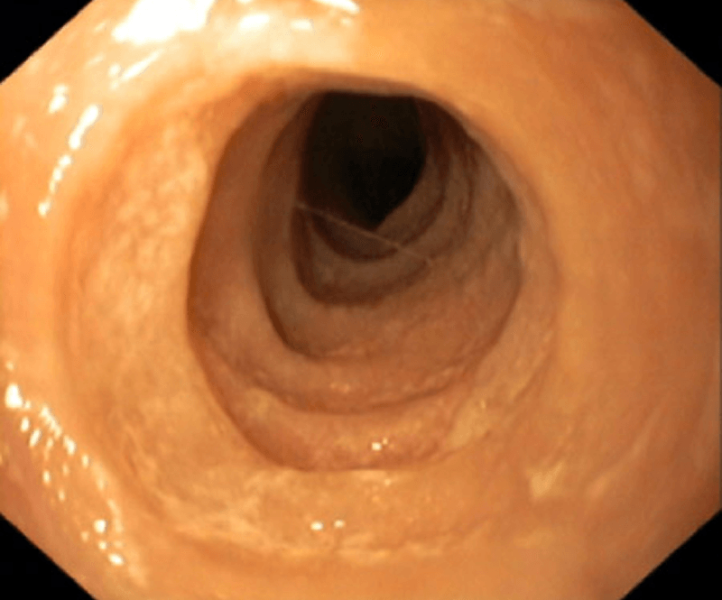
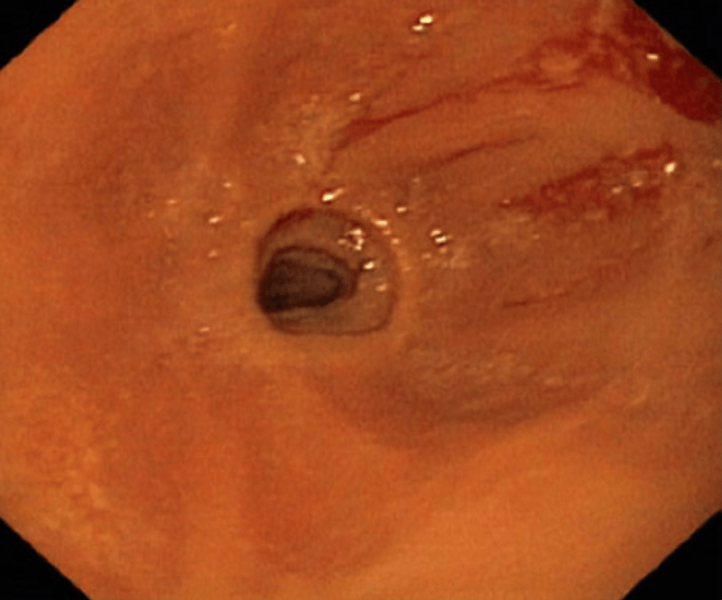
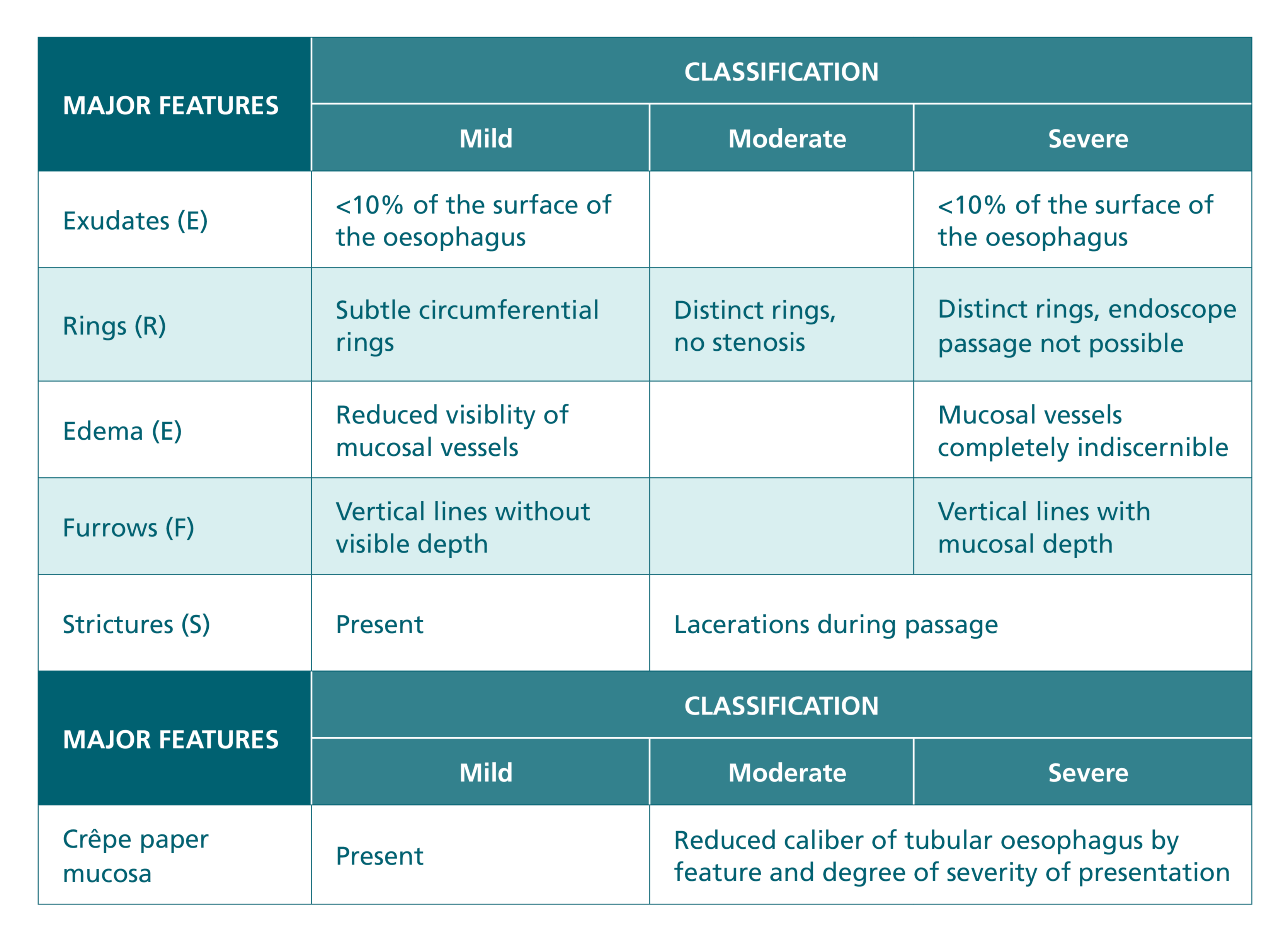
White exudates, longitudinal furrows, oedematous oesophageal mucosa with loss of vascular pattern, concentric rings (also called oesophageal trachealisation), and/or fragile (or crêpe paper) mucosa which bleeds easily, including during the passage of an endoscope, can be observed on endoscopy in a patient with oesophageal dysfunction, increasing the suspicion of the EoE, to be confirmed by biopsy (see Fig. 1).1
However, about 10-20% of patients with EoE have a normal oesophagus and thus it is important that all patients with oesophageal dysfunction have multiple biopsies collected regardless as to the appearance on endoscopy. Furthermore, because of the patchy nature of the disease in the oesophagus, multiple biopsies should be collected in all 3 segments, otherwise there’s a risk of missing the diagnosis7 (see Section 4 below).
The EoE Endoscopic Reference Score (EREFS) was developed to enable a standardised approach to the classification and the grading of severity of endoscopic features of EoE as detailed above. While the EREFS could be employed in clinical practice, it is used primarily as a research tool (see table 2).8
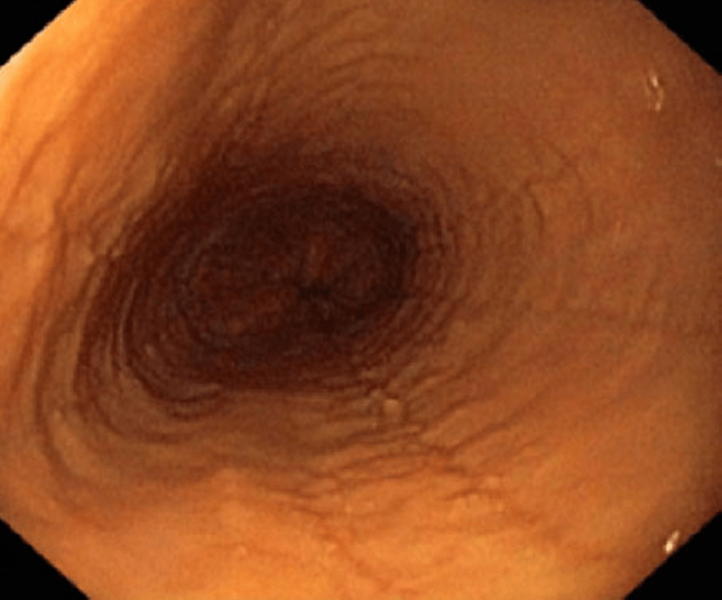
1. Furrows and oedema
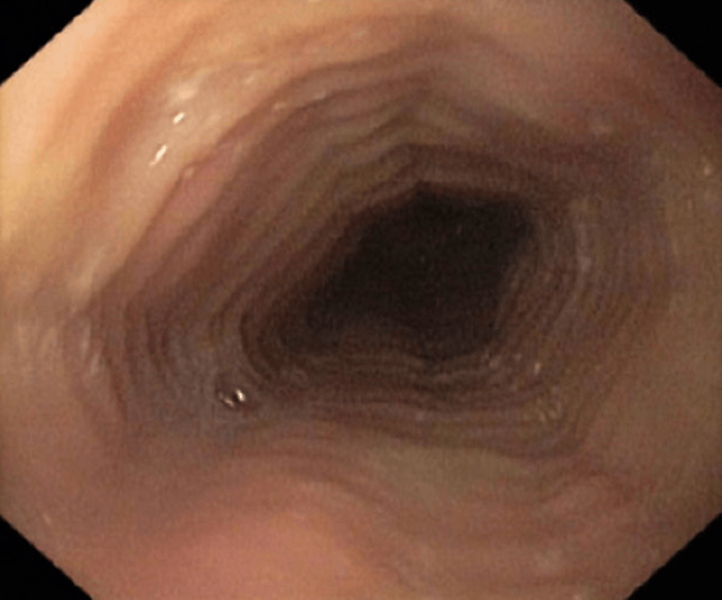
2. Rings and oedema
3. Rings (trachealisation), exudate, oedema
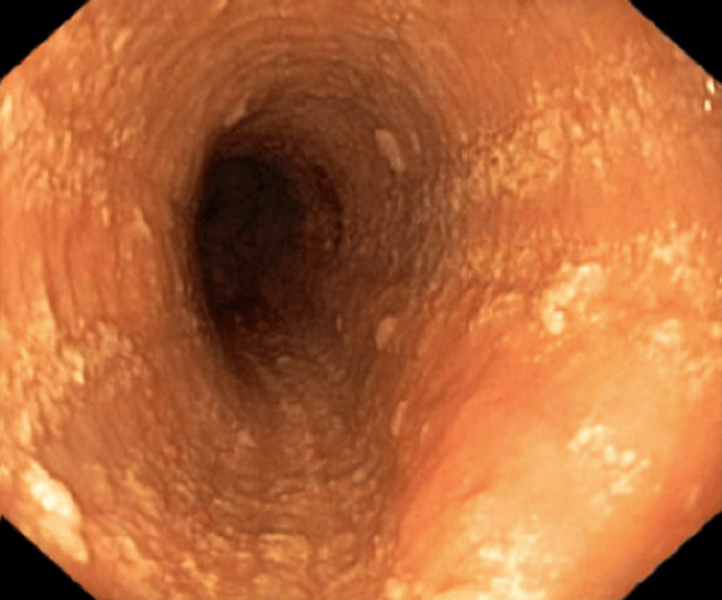
4. Exudate
5. Strictures (severe)
A diagnosis of EoE is confirmed if at least 15 eosinophils (eos) per high power field (hpf); corresponding to approximately 60 eos per mm2 hpf, are detected from at least 1 hpf in an oesophageal biopsy.
Due to the patchy nature of the pathology in EoE, at least six biopsies should be collected from different segments of the oesophagus (i.e. 2 each from the proximal, mid and distal segments), with the distal biopsy taken at least 5 cm above the gastroesophageal junction for histological testing. Biopsies should be collected from areas with prominent pathology but also from areas which appear to have normal mucosa on endoscopy, as 10–20% of EoE patients exhibit no visible alterations on endoscopy, as stated above. Biopsies should also be collected from the stomach and duodenum to rule out other causes of the eosinophilia in the oesophagus.1 Hematoxylin-eosin (HE) staining is sufficient for histological examination in routine clinical practice.
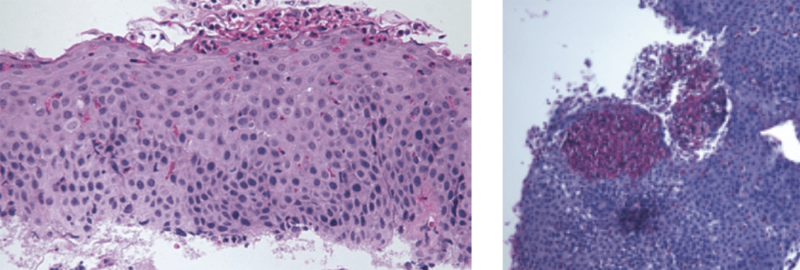
The validated Eosinophilic Oesophagitis Histologic Scoring System (EoEHSS) can be used to evaluate oesophageal biopsies in a standardised manner by incorporating the extent and severity of eight typical histological features (eosinophil density, basal zone hyperplasia, eosinophil-rich microabscesses, eosinophil surface layering, dilated intercellular spaces, surface epithelial alteration, dyskeratotic epithelial cells and lamina propria fibrosis).9 These might be included on the pathology report, however, again eosinophil count or density is the primary diagnostic marker for EoE. Notably, these microabscesses are observed on endoscopy as the white exudates described above and may be initially assumed by the endoscopist to be a fungal infection, only to be confirmed as these eosinophil-rich microabscesses by a pathologist when a biopsy is taken.
- Lucendo AJ, Molina-Infante J, Arias Á, von Arnim U, Bredenoord AJ, Bussmann C et al. Guidelines on eosinophilic oesophagitis: evidence-based statements and recommendations for diagnosis and management in children and adults. United European Gastroenterol J 2017; 5(3):335–58.
- Schoepfer AM, Straumann A, Panczak R, Coslovsky M, Kuehni CE, Maurer E et al. Development and validation of a symptom-based activity index for adults with eosinophilic oesophagitis. Gastroenterology 2014; 147(6):1255–66.e21.
- Dellon ES, Irani AM, Hill MR, Hirano I. Development and field testing of a novel patient-reported outcome measure of dysphagia in patients with eosinophilic oesophagitis. Aliment Pharmacol Ther 2013; 38(6):634–42.
- Martin LJ, Franciosi JP, Collins MH, Abonia JP, Lee JJ, Hommel KA et al. Pediatric Eosinophilic Oesophagitis Symptom Scores (PEESS v2.0) identify histologic and molecular correlates of the key clinical features of disease. J Allergy Clin Immunol 2015; 135(6):1519–28.e8.
- Franciosi JP, Hommel KA, Bendo CB, King EC, Collins MH, Eby MD et al. PedsQL eosinophilic oesophagitis module: feasibility, reliability, and validity. J Pediatr Gastroenterol Nutr 2013; 57(1):57–66.
- Miehlke S. Clinical features of eosinophilic oesophagitis in children and adults. Best Pract Res Clin Gastroenterol 2015; 29(5):739–48.
- Attwood S and Epstein J. Eosinophilic oesophagitis: recent advances and practical management. Frontline Gastroenterol. 2020; 12(7):644–64.
- Hirano I, Moy N, Heckman MG, Thomas CS, Gonsalves N, Achem SR. Endoscopic assessment of the oesophageal features of eosinophilic ooesophagitis: validation of a novel classification and grading system. Gut 2013; 62(4):489–95.
- Collins MH, Martin LJ, Alexander ES, Boyd JT, Sheridan R, He H et al. Newly developed and validated eosinophilic oesophagitis histology scoring system and evidence that it outperforms peak eosinophil count for disease diagnosis and monitoring. Dis Esophagus 2017; 30(3):1–8.